Using chemical peels on skin of colour

Chemical peels are used to create an injury of a defined skin depth with the aim to stimulate collagen and epidermal regeneration, enhancing the texture and appearance of the skin whilst creating a more evenly distributed melanin.1
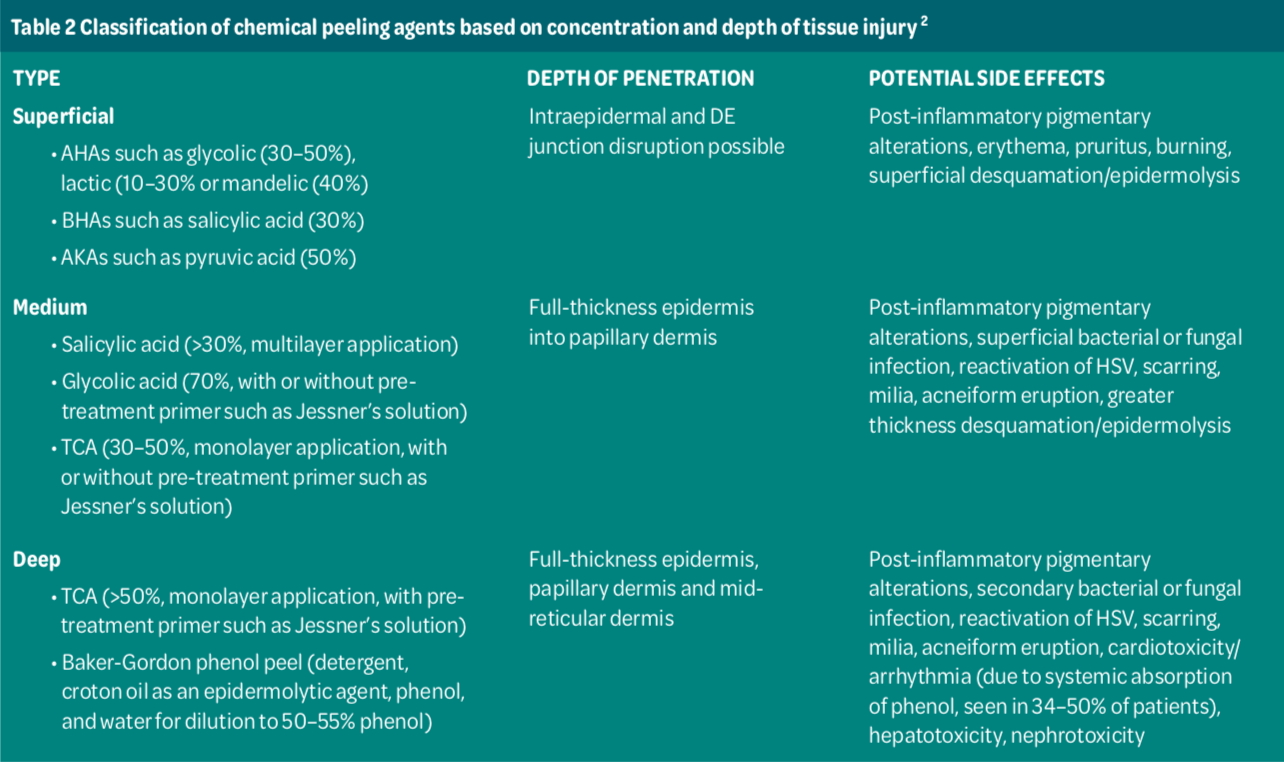
The benefits of chemical peels are numerous, with the prime goal to enhance the clinical appearance of the skin.2 They serve to address inflammatory and non- inflammatory acne lesions as well as acne scarring. They also manage pigmentary disorders such as photo-ageing and inflammatory dermatoses. In addition, they restore skin moisture, stimulate collagen and elastin, reduce the quantity and the quality of fine lines and wrinkles. In essence, they play an integral role in the overall skin rejuvenation and youthful appearance.3
The term peeling originates from the English word to peel = to come off in sheets or scales, to shed the outer layer, or to strip off.4
This process involves the application of a chemical agent to the skin leading to the controlled destruction of part or all of the
epidermis through chemexfoliation, which is then followed by an organised regeneration of the skin.2
A BRIEF HISTORY OF CHEMICAL PEELS
Chemexfoliation has been used for centuries to improve signs of ultraviolet light-induced sun damage.5
In fact, chemical peels have been used since ancient times and were first described in Egyptian medicine in 1150 BC. In ancient Egypt, Cleopatra used sour milk, which is now known to contain lactic acid. This practice was also described in ancient Greek and Roman literature.4
In 1874, Ferdinand Von Hebra, a dermatologist from Vienna, applied chemical peels for the treatment of melasma, whilst in 1882, in Hamburg, Paul G. Unna demonstrated the properties of salicylic acid, resorcinol, trichloroacetic acid (TCA) and phenol on the skin. The use of phenol was developed in France after the First World War.4
In the 1940s, Eller and Wolff from the United States provided the first systematic description of the use of phenol, salicylic
acid, resorcinol, and dry ice to treat scars. Whilst in England, Mac Kee applied the use of phenol to treat scars but did not publish his results until 1952.4
COMMON PEELING AGENTS IN AESTHETIC AND CLINICAL PRACTICE
Chemical peels are routinely applied in everyday practice to manage and maintain skin health and address skin disease. Commonly used acids include,
Alpha hydroxyl acids (AHA) such as lactic, glycolic, mandelic, to name a few. These acids provide humectant benefits, reduce hyper keratinisation, inhibit melanogenesis, and promote collagen synthesis in the skin. Mandelic acid has the added benefit of antibacterial properties and is therefore beneficial for acne-prone skin.6
Beta hydroxyl acids (BHAs), such as salicylic acid (SA), is an aromatic carboxylic acid that is lipophilic keratolytic in nature with the ability to dissolve follicular impactions, thereby reducing acne lesions. Its benefits are attributed to its effective anti-inflammatory and exfoliating properties.7
A derivative of SA, ß-lipo hydroxy acid (LHA, up to 10%) which provides chemexfoliation at lower concentrations with the added benefit of anti-inflammatory, antifungal and anticomedonic properties. LHA has an additional fatty acid chain which makes it more lipophilic than SA with regards to its mode of action and keratolytic effect. Therefore, it penetrates with ease into the sebaceous follicle but less deeply into the skin than glycolic or salicylic acid. In essence, it targets the follicle and the epidermis with a PH of 5.5, similar to normal skin; therefore, a more tolerable experience for the patient. Similar to SA, it is also self-neutralising.6
Pyruvic acid is an alpha-keto acid that delivers superficial exfoliating action similar to salicylic acid, with a lesser degree of lipophilicity. However, it is also partially hydrophilic, exhibiting features similar to glycolic acid. It is commonly applied as a superficial peeling agent for the treatment of inflammatory and comedonal acne but is not as effective as salicylic acid. It is used in the treatment of acne vulgaris and associated disorders of excess sebum production due to greater lipophilic property and ease of penetration through the lipid barrier. It is also used in the management of mild photo-ageing and superficial hyperpigmentation. Although pyruvic acid displays similar properties to salicylic acid, it is not self-neutralising and is similar to glycolic acid, where neutralisation is required.2
TCA is a caustic peeling agent that coagulates skin proteins. Observation during the treatment is vital when assessing the endpoint of action. The PH and the depth of penetration are concentration- dependent. Therefore, it becomes more acidic and penetrates deeper with increasing concentration. TCA is a versatile peeling agent commonly applied to improve fine lines, wrinkles, smooth skin texture, acne scarring, and the treatment of actinic keratosis and melasma.8
Retinol is converted to retinoic acid in the skin to encourage cellular turnover and normal desquamation whilst reducing
the incidence of corneocyte cohesion. Retinoids inhibit melanogenesis, stimulate collagen production, and discourage hyper keratinisation within the follicle. They also increase water content in the epidermis. Their overall advantage of being safe for all Fitzpatrick skin types I-VI is to stimulate the fibroblasts to produce additional collagen and elastin and address pigmentation by inhibiting melanosomes from being transferred from the melanocytes into the keratinocytes.2
Phenol is also known as carbolic acid or hydroxybenzene (C6H5OH), derived from coal tar. It is hydrophobic, aromatic alcohol, with cytotoxic, antiseptic, and analgesic properties. It functions as a protoplasmic poison by altering cell membranes, deactivating enzymes, and producing insoluble proteinates.8
Resorcinol is a caustic agent from the phenols group, with different properties. It serves as an exfoliant and is applied in the form of solutions or ointments, with concentrations ranging from 10-70%. It is also incorporated with other chemical peel preparations.4
The modified Jessner’s solution was the first documented blended acid peel with chemoexfoliating and keratolytic properties used for the treatment of acne, dyschromia, and extrinsic ageing. The modified Jessner’s solution is often administered due to its ease of use, lower risks and uniform depth with the advantage of being suitable for Fitzpatrick skin types I-VI.2
Other peeling agents include arbutin, L-ascorbic acid (vitamin C), azelaic acid, citric, tranexamic acid, glutathione, Kojic acid, lactic acid, phytic acid, where some have antioxidant properties and serve to suppress melanin production whilst promoting evenly distributed skin tone. 8
CLASSIFICATION OF CHEMICAL PEELS
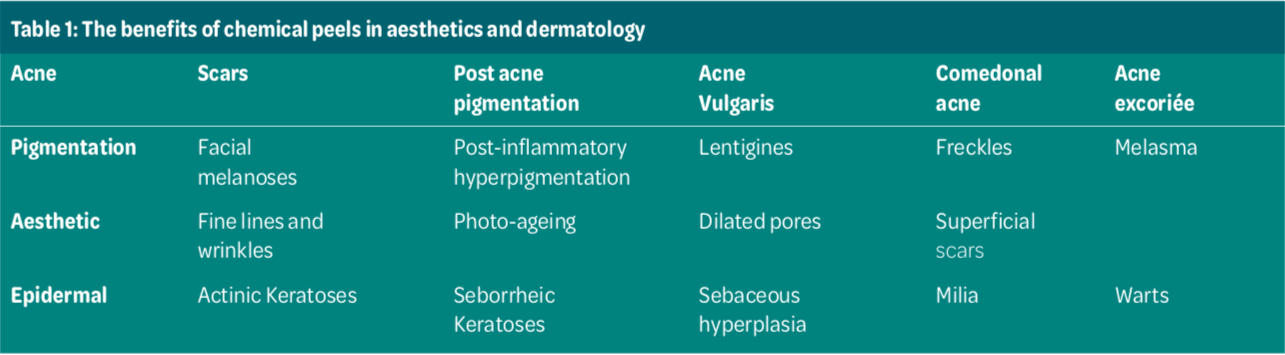
Chemical peels are classified by the depth of penetration and mode of action and treatment objective. Applying the appropriate depth determines the overall success of the treatment whilst minimising the risk of complications.6
Very superficial peels function to remove the stratum corneum at a depth of 0.06 mm, superficial peels induce epidermal exfoliation of the granular layer to basal layer at a depth of 0.45 mm, medium depth peels target the papillary dermis at a depth of 0.6 mm and deep peels penetrate the mid-reticular dermis at a depth of 0.8 mm.9
CLINICAL APPLICATIONS
Superficial peels are beneficial in the treatment of mild dyschromia, acne, post- inflammatory pigmentation. Epidermal regeneration is predicted between three to five days where desquamation is well tolerated. Their mode of action involves the reduction of corneocyte adhesion and an increase in dermal collagen. They serve to achieve radiant luminosity and overall rejuvenated skin.6
On the other hand, medium-depth peels are indicated in the treatment of dyschromia, such as solar lentigines, multiple keratoses, superficial scars, pigmentary disorders, and textural changes. The treatment involves a longer healing process where full epithelialisation is achieved in seven days.9
Deep peels are used to address photo- ageing, deep or coarse wrinkles, scars, and in some cases, precancerous skin lesions. Deep peels lead to denaturation of surface keratin and other proteins in the dermal and epidermal layers of the skin, making their journey to the reticular dermis with the objective to potentiate collagen regeneration. Epithelialization resumes within five to ten days, where significant healing time of two months or more may be required.6
Superficial peels are generally considered safe in skin of colour, while caution must be applied when considering medium depth peels. It is strongly advised that deep peels are not performed on skin of colour.9
However, it is always important to assess skin of colour through an in-depth consultation as what may be superficial can behave as medium depth, and therefore, patient selection and assessment are paramount.10
PEEL INTENSITY
There are a number of contributing factors to peel intensity. These include the status of the skin at the time of the treatment;
for example, is the skin prepped? It may be essential to prep or prime the skin, especially skin of colour, prior to treatment, with the use of ingredients such as hydroquinone, retinoid, vitamin C and sunscreen.9
Peel intensity may also be influenced by the amount of peel applied, the number of layers, the concentration used, the time left on the skin, the location and thickness of the area treated, for example, face or body.2
AHA: alpha hydroxy acid; BHA: beta hydroxyl acid; AKA: alpha-keto acid; TCA: trichloroacetic acid; DE: dermo- epidermal; HSV: herpes simplex virus Jessner’s solution: salicylic acid, 14g; resorcinol 14g; lactic acid (85%), 14g; and ethanol to 100mL; used as a primer to optimise medium-depth peels by disrupting cornified layer.

Balsam Alabassi is the founder of DermRefine Skin Clinic, Mayfair London. An Independent Prescriber and an advanced skin specialist with level 7 qualification in cosmetic injectables as well an NVQ level 4 in laser hair removal and advanced skin rejuvenation. With over 20 years of clinical pharmacy and leadership experience, her mission is to educate, enable and empower her patients to truly own their skin and skin health.
REFERENCES
1. El Samahy, M., Ghoz, M. and Ramzy, N., 1998. Effects of Combination Chemical Peel on Facial Photodamaged Skin. The American Journal of Cosmetic Surgery, 15(3), pp.263- 271.
2. Soleymani, T., Lanoue, J., & Rahman, Z. (2018). A Practical Approach to Chemical Peels: A Review of Fundamentals and Step-by-step Algorithmic Protocol for Treatment. The Journal of clinical and aesthetic dermatology, 11(8), 21–28.
3. O’Connor, A., Lowe, P., Shumack, S. and Lim, A., 2017. Chemical peels: A review of current practice. Australasian Journal of Dermatology, 59(3), pp.171-181.
4. Surgicalcosmetic.org.br. 2013. Review article Chemical peels: review and practical applications. [online] Available at:
5. Lee, K., Wambier, C., Soon, S., Sterling, J., Landau, M., Rullan, P. and Brody, H., 2019. Basic chemical peeling: Superficial and medium-depth peels. Journal of the American Academy of Dermatology, 81(2), pp.313-324
6. Rendon, M. I., Berson, D. S., Cohen, J. L., Roberts, W. E., Starker, I., & Wang, B. (2010). Evidence and considerations in the application of chemical peels in skin disorders and aesthetic resurfacing. The Journal of clinical and aesthetic dermatology, 3(7), 32–43.
7. Linder, J., 2013 Chemical Peels and Combination Therapies. Plastic Surgical Nursing, Volume 33 Number 2. pp 88 - 91.
8. Rullan, P. and Karam, A., 2010. Chemical Peels for Darker Skin Types. Facial Plastic Surgery Clinics of North America, 18(1), pp.111-131.
9. Khunger, N., 2008. Standard guidelines of care for chemical peels. [online] Indian Journal of Dermatology, Venereology and Leprology. Available at:
10. Clark, E. and Scerri, L., 2008. Superficial and medium-depth chemical peels. Clinics in Dermatology, 26(2), pp.209-218.